
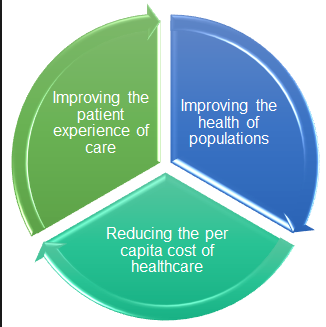
As you likely know, we are in the middle of healthcare reform. Our healthcare delivery is changing with three main goals as the driving force: improve quality, improve outcomes, and reduce cost — the Triple Aim (2). Telehealth and mHealth have been embraced by many as potential solutions — innovative deviations from the traditional ideas of healthcare. However, state and federal policy formation, implementation, and modification have been slow and ineffective inhibiting the full adoption of telehealth (2). The inconsistent, unclear policy and regulation and insufficient resources have sparked action and advocacy from various players in the telehealth world.
Solid evidence, consumer demand, leadership, commitment, and technology advancements are critical in optimizing telehealth services (2). Large organizations such as Nebraska Medicine, Kaiser Permanente, or Mayo Clinic play a vital role in meeting these demands by designing, implementing, and evaluating telehealth projects. It is pilot studies like those developed at these organizations that provide this solid evidence, demonstrate leadership, and make the consumer demands known.



Special interest groups such as the American Telemedicine Association (ATA) and the International Society for Telemedicine & eHealth also play a fundamental role in challenging outdated ideas of healthcare delivery, advocating for change, and providing insight and recommendations to policymakers.
Another important supporter of telehealth is the Center for Connected Health Policy (CCHP); a nonprofit, nonpartisan organization that acts as a catalyst for change by bringing policymakers together with private health care sector, health plans, academic researchers, and consumer health advocates to gain ground in the Triple Aim objectives through telehealth (1).
These groups provide expert opinions to executive branches of government such as the Department of Health and Human Services (DHHS) where policy is designed, rules are made, the policy is put into operation, and subsequently evaluated (3). In an interview with Senator Nicole Fox, a committee member of the DHHS, she discussed the reliance that committee members have on expert advocate groups to inform them of the current status of telehealth and the future needs. Senator Fox provided examples of committee members not understanding the clinical pathways for many diagnoses, what services are appropriate for telehealth delivery, or what types of medical technology are available and how they can be useful to patients and providers. It is often difficult for government representatives and stakeholders such as CMS to see beyond the upfront costs of telemedicine; it is because of this that solid evidence is so vital in order to make forward progress (Senator Nicole Fox, personal communication, February 9, 2016).
Regulatory Mechanisms
Some of the most commonly debated regulatory efforts include reimbursement rates, limited services, cross-state licensure, and distance between provider and patient among others. Nebraska has been quite progressive in the expansion of telehealth. LB 1076 – the Nebraska Telehealth Act addressed many of the issues other states continue to battle (4). They have:
- revised the definition of telehealth to include telemonitoring and medical information electronically exchanged from one site to another whether synchronously or asynchronously (i.e. store and forward messaging through secured email is reimbursable)
- expanded the eligible telehealth providers to include all Medicaid enrolled providers
- clarified that a relationship can be established between patient and provider without a face-to-face visit
- required managed care contracts with managed care plans to include coverage of healthcare services delivered through telehealth.
There are plenty of regulatory mechanisms that continue to be debated — interstate licensure (expedited multi-state licensure), parity laws for private insurance coverage (see image below for U.S. report card), expansion of covered diagnoses, and more. These issues will need to be addressed in a timely manner if telehealth is to be fully adopted and available to everyone in need of access to care. Unfortunately, regulatory mechanisms need to be updated as frequently as the technology itself. Thankfully, there are a lot of actors advocating for the cause.

While changing public and private policy is important in advancing telehealth, it is “insufficient for achieving widespread adoption of telehealth care” (2). Institutions and special interest groups are integral in creating partnerships in research, practice, technology, consumer support, policy, and financing.
References:
Center for Connected Health Policy (CCHP). (2016). About CCHP. Retreived from http://cchpca.org/about-cchp
Gutierrez, M. (2014). The role of telehealth in the triple aim. Retrieved from http://www.phi.org/news-events/655/the-role-of-telehealth-in-the-triple-aim
Longest, B.B. Jr. (2016). Health policymaking in the United States (6th ed.). Chicago, IL: Health Administration Press.
Nebraska Legislature. (2014). Legislative bill 1076. Retrieved from http://nebraskalegislature.gov/FloorDocs/103/PDF/Slip/LB1076.pdf
Thank you for your informative blog information! I think telehealth is a very exciting new healthcare solution for our future. I agree, as we continue to move forward in this new age of healthcare reform it is inevitable that we will need to find better ways to provide health for the growing number of newly insured people. Incorporating telehealth more frequently to accommodate the growing healthcare needs of the population while maintaining the Triple Aim objectives is certainly an exceptional opportunity (Gutierrez, 2014). I have been fortunate to be part of a team related to my evidence base project that is looking at utilizing telehealth as an extension for healthcare management of heart failure patients. Dignity Health of Sacramento California currently uses telehealth for several purposes, which have been very successful especially for homecare, cardiology, and stroke (Dignity Health, n.d.). The newly established Center for Transitional Care in Arizona is in the process of developing a program that will be similar to the one in Sacramento. I think we will start seeing more and more telemedicine offered from major healthcare centers and providers as time goes on when more information is available regarding health and cost benefits.
It is not shocking to hear that the state and federal policy formation is slow, but encouraging to know there are several key players that are well versed to assist with progression of the process. As I looked more into Arizona’s role with telehealth, I was excited to learn our legislature were pioneers for introducing telemedicine. The Arizona Telemedicine Program was established in 1996 when Legislation granted $1.2 million for the University of Arizona Health and Sciences Center to pilot a telemedicine network (Arizona State Legislature, 2014). This program launched the first network of telemedicine in Arizona at eight different sites, which consisted of a state prison, six rural medical centers, and a hospital on an Indian reservation (Arizona State Legislature, 2014). The astounding successes of the program allowed for significant growth of telemedicine throughout the state and in 2005 federal funds were provided to the University of Arizona to create the Institute for Advanced Telemedicine and Telehealth (Arizona State Legislature, 2014). Additional movement by Legislation occurred with the passing of S.B 1353 in 2013, which is a parity bill that applied to rural areas and required private insurance to pay for services from telemedicine that would normally be covered for an in-person visit (Arizona State Legislature, 2014).
References
Arizona State Legilature. (2014). Retrieved from http://www.azleg.gov/briefs/Senate/TELEMEDICINE.pdf
Dignity Health. (n.d.). Retrieved from http://www.dignityhealth.org/sacramento/services/telehealth-network/?fullsite=1
Gutierrez, M. (2014). The role of telehealth in the triple aim. Retrieved fromhttp://www.phi.org/news-events/655/the-role-of-telehealth-in-the-triple-aim
LikeLike